Overview
Coronary Artery Disease (CAD) is a common yet serious condition in which the arteries supplying blood to the heart become narrowed or blocked due to the buildup of plaque. This plaque, also known as atherosclerosis, consists of cholesterol, calcium, fibrin, and cellular waste products. Over time, plaque can harden, leading to restricted blood flow to the heart muscle, which can have severe consequences.
The heart requires a constant supply of oxygen-rich blood to function effectively. When the coronary arteries become constricted, the heart muscle does not receive enough oxygen, leading to various cardiac complications. Some of the significant outcomes of CAD include angina (chest pain), myocardial infarctions (heart attacks), and heart failure.
- Angina: This is typically experienced as discomfort or pressure in the chest, often triggered by physical exertion or stress. It indicates that the heart is not getting enough oxygen due to reduced blood flow.
- Heart Attack (Myocardial Infarction): This life-threatening event occurs when a plaque ruptures, forming a blood clot that completely blocks the artery. Without prompt treatment, this can lead to severe damage to the heart muscle, arrhythmias, heart failure, or even death.
- Heart Failure: CAD can also lead to heart failure, a condition where the heart cannot pump sufficient blood to meet the body’s needs, often resulting from long-term damage or repeated heart attacks.
Risks
Several factors increase the risk of developing CAD, many of which are preventable or manageable. Key risk factors include:
- High Cholesterol Levels resulting in hyperlipidemia
- Smoking
- Diabetes
- High Blood Pressure resulting in hypertension
- Obesity
- Physical Inactivity
- Family History of Heart Disease
- Psychosocial Stress
These risk factors collectively account for nearly 90% of heart attacks, highlighting the importance of managing them to prevent or control CAD.
Symptoms
In its early stages, CAD may be asymptomatic. As the condition progresses, symptoms may include:
- Chest Pain or Discomfort (Angina)
- Shortness of Breath
- Fatigue
- Irregular Heartbeat
Diagnosing CAD involves a thorough review of medical history, physical examination, and various diagnostic tests. These tests help determine the extent and severity of the disease, including:
- Electrocardiogram (ECG or EKG): This test records the electrical activity of the heart to detect abnormalities.
- Stress Test with Echocardiography or Thallium Scintigraphy: These tests evaluate the heart’s function under physical exertion, often with ECG or imaging techniques to identify areas of the heart that may not receive adequate blood supply during exercise.
- CT Coronary Angiography: This non-invasive imaging test uses CT- Computed Tomography- technology and contrast material to visualize the coronary arteries.
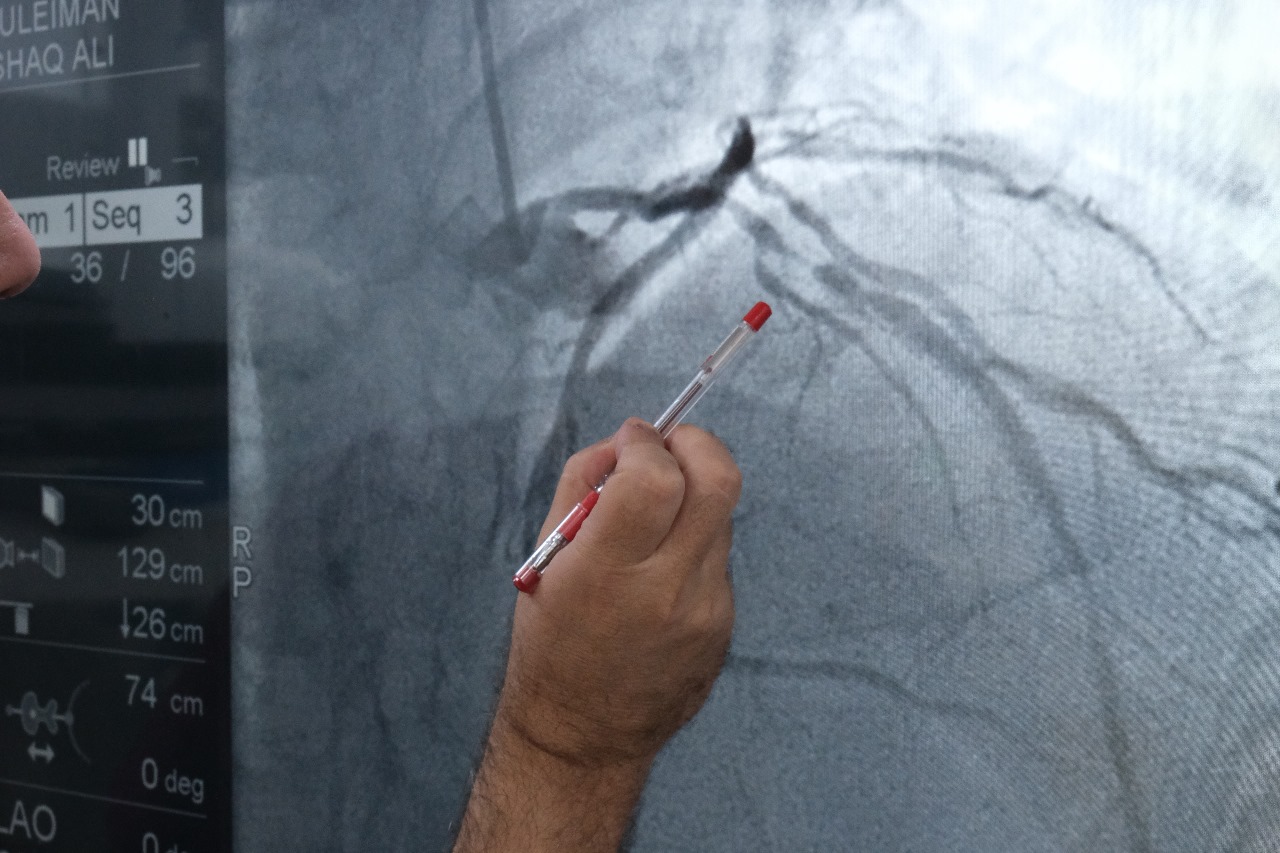
- Coronary Angiography: Considered the gold standard, this invasive procedure involves injecting dye into the coronary arteries to visualize blockages under X-ray via a catheter.
Treatment
Treatment for CAD is tailored to the severity of the disease and the individual patient’s symptoms. It typically includes:
- Lifestyle Modifications: Dietary changes, regular exercise, and smoking cessation are critical for managing CAD.
- Medications: These may include statins to manage cholesterol, antihypertensives to control blood pressure, and antiplatelets to prevent blood clots.
- Percutaneous Coronary Intervention (PCI): This minimally invasive procedure, often involving stent placement, is used to open blocked arteries, especially during acute heart attacks.
- Coronary Artery Bypass Graft (CABG): This surgical procedure is recommended for severe cases, involving the use of a graft to bypass blocked arteries.
If you have concerns about your heart health, it is essential to consult a cardiologist. Dr. Turquieh, with over 25 years of experience and thousands of successful interventions, is well-equipped to provide expert care for patients with CAD.

